Pelvic Cancers
Content Coming Soon…..
Content Coming Soon…..
A cyst is a closed pocket or pouch of tissue. It can be filled with air, fluid, pus, or other material. A vaginal cyst is a closed sac on or under the vaginal lining.
There are several types of vaginal cysts.
Vaginal cysts usually do not cause symptoms, although there may be a soft lump felt in the vaginal wall or protruding from the vagina. Cysts range in size from the size of a pea to that of an orange. Some women with vaginal cysts may have discomfort during sex or trouble inserting a tampon.
Upon pelvic examination, a mass or bulge of the vaginal wall may be seen or felt by the examiner. A biopsy may be necessary to rule out vaginal cancer, especially if the mass appears to be solid. If the cyst is located under the bladder or urethra, X-rays may be required to be sure the cyst does not involve these structures.
The only treatment needed may simply involve routine exams and watching the cyst for growth and other changes. Opening and draining the cyst does not usually work well and may lead to infection. Surgery may be needed if the cyst is causing symptoms. However, this can sometimes be a very involved surgery and is not recommended unless you are having more severe symptoms.
There are usually no complications from the cysts themselves. A surgical excision procedure carries a small risk of complications depending on where the cyst is located in relation to other structures.
The Bartholin’s glands are located at the entrance to a woman’s vagina, one on each side. They are small and cannot be seen or felt when they are normal. Their function is to secrete fluid onto the mucosal (inner) surface of the labia-the liplike skin surrounding the vagina. Problems with the Bartholin’s glands include cysts, which are relatively painless enlargements of the gland, and abscesses, which are infections of the gland. Typically only 1 of the 2 glands is affected.
A Bartholin’s cyst develops when the duct exiting the Bartholin’s gland becomes blocked. The fluid produced by the gland then accumulates, causing the gland to swell and form a cyst. An abscess occurs when a cyst becomes infected. Bartholin’s abscesses can be caused by any of a number of bacteria. These include bacterial organisms that cause sexually transmitted diseases such as chlamydia and gonorrhea as well as bacteria normally found in the intestinal tract, such as Escherichia coli. It is common for these abscesses to involve more than one type of organism.
A Bartholin’s cyst causes swelling of the labia on one side, near the entrance to the vagina. A cyst is usually not very painful, and significant pain suggests that an abscess has developed. However, large cysts may be painful simply by virtue of their size. A Bartholin’s abscess causes significant pain in addition to the swelling. The swollen area is extremely tender and the skin reddened. Walking and sitting may be quite painful. Women with Bartholin’s abscesses do not usually have fever. Vaginal discharge may be present, especially if the infection is caused by a sexually transmitted organism.
With Bartholin’s cysts and abscesses, the primary reason to seek emergency care is acute pain. Women who are experiencing severe pain or who cannot sit or walk comfortably should see a doctor as soon as possible.
Treatment is not always needed
If you have a small cyst that causes no symptoms, and does not become infected, then it may be best simply to leave it alone. However, always report a ‘lump’ in the area around your vagina (your vulva) to your doctor. Do not just assume a small lump is a Bartholin’s cyst. It is best for a doctor to examine you to confirm the diagnosis and to rule out other causes of lumps in the vulva. If a cyst causes symptoms, then it can be treated. A Bartholin’s abscess will almost always need treatment as it can be very painful. However, if an abscess is left long enough it is likely to burst and then may resolve without treatment. This is not recommended though as it will be very painful and you could become quite ill.
Antibiotics for an infection or abscess
A course of antibiotics has a good chance of curing an infected gland or abscess. However, as a rule, the more pus that forms, the larger the abscess, and the less chance that antibiotics alone will be sufficient to clear the abscess without also needing to drain the pus.
Surgery for Bartholin’s Cyst or Abscess
The main aim of the operation is to drain any fluid or pus. This relieves symptoms. But also, another aim is to minimise the chance of the problem recurring.
Marsupialisation
A small operation called marsupialisation is the traditional treatment used to treat a Bartholin’s cyst or abscess. A small cut (incision) is made into the cyst or abscess just inside the entrance to the vagina. Any fluid or pus drains out. The cut is widened to about 1 cm. A few stitches are then used to to stitch the inside lining of the cyst to the overlying skin. This then creates a small new permanent opening for fluid to drain out of the gland. Initially, the opening that is left is like a pouch – hence the name of the operation. However, the opening gradually becomes smaller and soon the opening becomes tiny and not noticeable. But this new opening is, in effect, like a new duct which allows any fluid that is made by the gland to drain. A course of antibiotics may be prescribed if pus is drained from an abscess. However, antibiotics are not always needed once the pus has been drained. Marsupialisation is usually successful. In only a few cases does the problem recur if this procedure is done. If a simple cut is made to drain the fluid or pus without then doing a marsupialisation, there is a higher chance that the problem will recur at some point. As with all operations there is a small chance of problems. For example, infection of the wound occurs in a small number of cases following marsupialisation.
Sometimes the entire gland is removed by a surgical operation. This is considered a ‘last resort’ but may be advised if you have several recurrences of a Bartholin’s cyst or abscess.
Prevention of Bartholin’s cysts or Abscesses
It is not usually possible to prevent a Bartholin’s Cyst or Abscess. Most occur ‘out of the blue’ for no apparent reason. Some Bartholin’s abscesses are due to sexually transmitted infections, and so using a condom when having sex may prevent some cases. As mentioned, some people say that, if a cyst develops, then sitting in warm baths may possibly help it to burst and prevent a possible abscess from developing.
Cervical cancer (cancer of the cervix) is cancer of the neck of the womb. The cervix is the lower part of the uterus (womb) which extends slightly into the top of the vagina. Most cases develop in women in their 40s to 60s. If cervical cancer is diagnosed at an early stage, there is a good chance of a cure. Regular cervical screening tests can detect ‘pre-cancer’ which can be treated before cancer develops
A narrow passage called the cervical canal (or endocervical canal) goes from the vagina to the inside of the uterus. This is normally kept quite tightly shut, but allows blood to flow out from the uterus during a period, and sperm to travel inside if you have sex. It opens very wide during labour if you have a baby. The surface of the cervix is covered with skin-like cells. There are also some tiny glands in the lining of cervical canal which make mucus.
There are two main types of cervical cancer:
Cervical cancer is the second most common type of cancer in women in the UK. It kills just over 1,000 women every year in the UK. However, the number of cases diagnosed each year has fallen over recent years. This is because cervical cancer can be prevented by regular cervical screening tests (see Cervical Screening and Colposcopy).
In the case of cervical cancer, the cancer develops from a cell which is already abnormal. In most cases, abnormal cells are present for years before one of the abnormal cells becomes cancerous and starts to multiply out of control into a cancerous tumour. The initial ‘pre-cancerous’ abnormality of cervical cells is usually caused by a prior infection with the human papilloma virus.
There are many strains of HPV. Two types, HPV 16 and 18, are involved in the development of most cases of cervical cancer. (Note: some other strains of HPV cause common warts and verrucas. These strains of HPV are not associated with cervical cancer.) The strains of HPV associated with cervical cancer are nearly always passed on by having sex with an infected person. An infection with one of these strains of HPV does not usually cause symptoms. So, you cannot tell if you or the person you have sex with are infected with one of these strains of HPV.
In some women, the strains of HPV that are associated with cervical cancer affect the cells of the cervix. This makes them more likely to become abnormal which may later (usually years later) turn into cancerous cells. Note: within two years, 9 out of 10 infections with HPV will clear completely from the body. This means that most women who are infected with these strains of HPV do not develop cancer.
The HPV vaccine has recently been introduced for girls from the age of 12 in the UK. Studies have shown that the HPV vaccine is very effective at stopping cancer of the cervix developing. The vaccine has been shown to work better for people who are given the vaccine when they are younger, before they are sexually active, compared to when it is given to adults. However, even if you have had the HPV vaccine you must attend for cervical screening. This is because the vaccine does not guarantee complete protection against cervical cancer.
Other factors that increase the risk of developing cervical cancer include the following:
You may have no symptoms at first when the tumour is small. As the tumour becomes larger, in most cases the first symptom to develop is abnormal vaginal bleeding such as:
An early symptom in some cases is a vaginal discharge that smells unpleasant, or discomfort or pain during sex. All of the above symptoms can be caused by various other common conditions. But if you develop any of these symptoms, you should have it checked out by a doctor. In time, if the cancer spreads to other parts of the body, various other symptoms can develop.
For further information on Cancer of the Cervix, please visit:
http://www.patient.co.uk/health/Cancer-of-the-Cervix.htm#section_3
Uterine fibroids are the most common non-cancerous tumors in women of childbearing age. They are benign tumours that originate in the uterus (womb). Although they are composed of the same smooth muscle fibres as the uterine wall (myometrium), they are many times denser than normal myometrium. Uterine fibroids are usually round or semi-round in shape. The cause of fibroids is unknown. Risk factors include being of Afro-Caribbean origin or being overweight.
We do not know exactly why women develop these tumours. Genetic abnormalities, alterations in growth factor (proteins formed in the body that direct the rate and extent of cell proliferation) expression, abnormalities in the vascular (blood vessel) system, and tissue response to injury have all been suggested to play a role in the development of fibroids.
Family history is a key factor, since there is often a history of fibroids developing in women of the same family. Race also appears to play a role. Women of African descent are two to three times more likely to develop fibroids than women of other races. Women of African ancestry also develop fibroids at a younger age and may have symptoms from fibroids in their 20s, in contrast to Caucasian women with fibroids, in whom symptoms typically occur during the 30s and 40s. Pregnancy and taking oral contraceptives both decrease the likelihood that fibroids will develop. Fibroids have not been observed in girls who have not reached puberty, but adolescent girls may rarely develop fibroids. Other factors that researchers have associated with an increased risk of developing fibroids include having the first menstrual period (menarche) prior to age 10, consumption of alcohol (particularly beer), uterine infections, and elevated blood pressure (hypertension).
Oestrogen tends to stimulate the growth of fibroids in many cases. During the first trimester of pregnancy, up to 30% of fibroids will enlarge and then shrink after the birth. In general, fibroids tend to shrink after menopause, but postmenopausal hormone therapy may cause symptoms to persist.
Overall, these tumours are fairly common and occur in up to 50% of all women. Most of the time, uterine fibroids do not cause symptoms or problems, and a woman with a fibroid is usually unaware of its presence
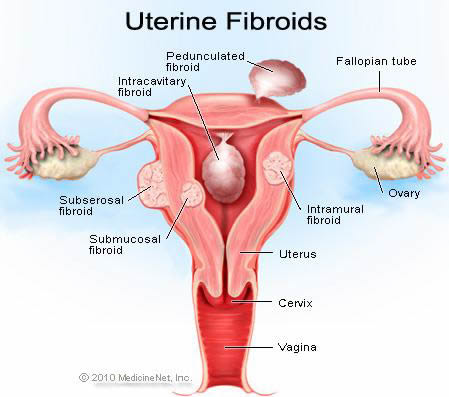
Uterine fibroids are often described based upon their location within the uterus. Subserosal fibroids are located beneath the serosa (the lining membrane on the outside of the organ). These often appear localized on the outside surface of the uterus or may be attached to the outside surface by a pedicle. Submucosal (submucous) fibroids are located inside the uterine cavity beneath the lining of the uterus. Intramural fibroids are located within the muscular wall of the uterus.
Most women with uterine fibroids have no symptoms.
However, abnormal uterine bleeding is the most common symptom of a fibroid. If the tumors are near the uterine lining, or interfere with the blood flow to the lining, they can cause heavy periods, painful periods, prolonged periods or spotting between menses. Women with excessive bleeding due to fibroids may develop iron deficiency anaemia. Uterine fibroids that are deteriorating can sometimes cause severe, localized pain.
Fibroids can also cause a number of symptoms depending on their size, location within the uterus, and how close they are to adjacent pelvic organs. Large fibroids can cause:
While fibroids do not interfere with ovulation, some studies suggest that they may impair fertility and lead to poorer pregnancy outcomes. In particular, submucosal fibroids that deform the inner uterine cavity are most strongly associated with decreases in fertility.
The following are the signs that can suggest fibroids
Treatment depends on several things, including:
Some women may just need pelvic exams or ultrasounds every once in a while to monitor the fibroid’s growth.
Non-surgical techniques are usually hormonal in nature and include the use of drugs that turn off the production of oestrogen from the ovaries (GnRH analogs). These medications are given for three to six months and induce a hypoestrogenic (low oestrogen) state. When successful, they can shrink the fibroids by as much as 50%. Side effects of these drugs are similar to the symptoms of the peri-menopause and can include hot flashes, sleep disturbance, vaginal dryness, and mood changes. Bone loss leading to osteoporosis after long-term (12+ months) use is the most serious complication. These drugs may also be used as preoperative treatment prior to undergoing surgical treatment of leiomyoma (fibroids).
Mifepristone is an antiprogestin drug that can shrink fibroids to an extent comparable to treatment with the GnRH analogs. This drug, sometimes known as the “morning-after pill” is also used to terminate early pregnancy. Treatment with mifepristone also reduced the bleeding associated with fibroids, but this treatment can be associated with adverse side effects such as overgrowth (hyperplasia) of the endometrium (uterine lining). Mifepristone is not approved by the US Food and Drug Administration (FDA) for the treatment of uterine leiomyomas, and the required dosages (different from those used for termination of early pregnancy) have not been determined.
Danazol is an androgenic steroid hormone that has been used to reduce bleeding in women with fibroids, since this drug causes menstruation to cease. However, danazol does not appear to shrink the size of fibroids. Danazol is also associated with significant side effects, including weight gain, muscle cramps, decreased breast size, acne, hirsutism (inappropriate hair growth), oily skin, mood changes, depression, decreased high density lipoprotein (HDL or ‘good cholesterol’) levels, and increased liver enzyme levels.
The administration of raloxifene (Evista) (a drug used to prevent and treat osteoporosis in postmenopausal women) has been shown to decrease the size of fibroids in postmenopausal women, but results with this therapy in premenopausal women have been conflicting.
Low dose formulations of oral contraceptives are also sometimes given to treat the abnormal bleeding associated with fibroids, but these do not shrink the fibroids themselves. Use of oral contraceptive pills has been associated with a decreased risk of developing fibroids, so some women may benefit from their use for this purpose
There are many ways of managing uterine fibroids. Surgical methods are the mainstay of treatment when treatment is necessary. Possible surgical interventions include Hysterectomy, or removal of the uterus (and the fibroids with it). Myomectomy is the selective removal of just the fibroids within the uterus. Myomectomy can be done through a laparoscope or with the standard open incision on the abdominal wall. Some treatments have involved boring holes into the fibroid with laser fibers, freezing probes (cryosurgery), and other destructive techniques that do not actually remove the tissue but try to destroy it in place. Surgery is necessary if there is suspicion of malignancy in any case of leiomyoma or uterine mass.
Another technique for treating fibroids is known as Uterine Artery Embolization (UAE). This technique uses small beads of a compound called polyvinyl alcohol, which are injected through a catheter into the arteries that feed the fibroid. These beads obstruct the blood supply to the fibroid and starve it of blood and oxygen. While this technique has not been in use long enough to evaluate long-term effects of UAE versus surgery, it is known that women undergoing UAE for fibroids have a shorter hospital stay than those having surgery but a greater risk of complications and readmissions to the hospital. Studies are underway to evaluate the long-term outcomes of UAE as opposed to surgical treatment. Uterine artery occlusion (UAO), which involves clamping the involved uterine arteries as opposed to injecting the polyvinyl alcohol beads, is currently under investigation as a potential alternative to UAE.
Uterine fibroids are identified in about 10% of pregnant women. Some studies have shown an increased risk of pregnancy complications in the presence of fibroids, such as first trimester bleeding, breech presentation, placental abruption, and problems during labour. Fibroids have also been associated with an increased risk of caesarean delivery. The size of the fibroid and its precise location within the uterus are likely to be important factors in determining whether a fibroid causes obstetric complications.
For the most part, uterine fibroids that do not cause a problem for the woman can be left untreated. In some cases, even fibroids that are not causing symptoms require removal or at least close observation. Rapid growth is a reason to watch more carefully, since a rare cancerous form of fibroid (referred to as a leiomyosarcoma) is usually a fast-growing tumour, and it cannot be differentiated from a benign fibroid by ultrasound, MRI , or other imaging studies. However, this type of tumour occurs in less than 1% of uterine fibroids.
Another risk of leaving these tumours alone is that they sometimes grow to a size that eventually cause significant symptoms, thus requiring removal. If fibroids grow large enough, the surgery to remove them can become more difficult and risky. Occasionally, fibroids are the cause of recurrent miscarriages. If they are not removed in these cases, the woman may not be able to sustain a pregnancy
Complications of untreated fibroids may also include:
In rare cases, fibroids may cause infertility. Fibroids may also cause complications if you become pregnant, although the risk is thought to be small:
Uterine Artery Embolisation (UAE) is a minimally invasive procedure that can be carried out through a small tube inserted into your groin. Through this tube, small plastic beads are injected into the arteries supplying blood to the fibroid. This blocks the arteries and causes the fibroid to shrink over the subsequent six months.
People who have UAE may suffer pain after the blood supply is removed, and strong painkillers are needed for about eight hours. There are some other complications that your specialist will be able to tell you about.
The advantage of UAE is that:
Further research needs to be carried out into the success rate of pregnancy after UAE. Sometimes, further embolisations or other procedures are needed after UAE. Your specialist will discuss this with you.
Sometimes, the fibroids can be removed using a surgical procedure known as a myomectomy. However, the operation is not suitable for every type of fibroid. Your gynaecologist (specialist in the female reproductive system) will be able to tell you whether a myomectomy is possible and what the complications are.
When they are possible, myomectomies are very effective operations. However, in a quarter to a third of all people who have a myomectomy, the fibroids grow back again.
Ovarian cysts are small fluid-filled sacs that develop in a woman’s ovaries. Most cysts are harmless, but some may cause problems such as rupturing, bleeding, or pain; and surgery may be required to remove the cyst(s). It is important to understand the function of the ovaries and how these cysts may form. Women normally have two ovaries that store and release eggs. Each ovary is about the size of a walnut, and one ovary is located on each side of the uterus. One ovary produces one egg each month, and this process starts a woman’s monthly menstrual cycle. The egg is enclosed in a sac called a follicle. An egg grows inside the ovary until estrogen (a hormone), signals the uterus to prepare itself for the egg. In turn, the lining of the uterus begins to thicken and prepare for implantation of a fertilized egg resulting in pregnancy. This cycle occurs each month and usually ends when the egg is not fertilized. All contents of the uterus are then expelled if the egg is not fertilized. This is called a menstrual period.
Ovarian cysts affect women of all ages. The vast majority of ovarian cysts are considered functional (or physiologic). This means they occur normally and are not part of a disease process. Most ovarian cysts are benign, meaning they are not cancerous, and many disappear on their own in a matter of weeks without treatment. While cysts may be found in ovarian cancer, ovarian cysts typically represent a harmless (benign) condition or a normal process. Ovarian cysts occur most often during a woman’s childbearing years. The most common types of ovarian cysts are the following:
Follicular cyst: This type of simple cyst can form when ovulation does not occur or when a mature follicle involutes (collapses on itself). A follicular cyst usually forms at the time of ovulation and can grow to about 2.3 inches in diameter. The rupture of this type of cyst and release of the egg can create sharp severe pain on the side of the ovary on which the cyst appears. This sharp pain (sometimes called Mittelschmerz) occurs in the middle of the menstrual cycle, during ovulation. About one-fourth of women with this type of cyst experience pain. Usually, these cysts produce no symptoms and disappear by themselves within a few months.
Corpus luteum cyst: This type of functional ovarian cyst occurs after an egg has been released from a follicle. After this happens, the follicle becomes what is known as a corpus luteum. If a pregnancy doesn’t occur, the corpus luteum usually breaks down and disappears. It may, however, fill with fluid or blood and persist on the ovary. Usually, this cyst is found on only one side and produces no symptoms.
Hemorrhagic cyst: This type of functional cyst occurs when bleeding occurs within a cyst.
Symptoms such as abdominal pain on one side of the body may be present with this type of cyst.
Dermoid cyst: This is a type of benign tumor sometimes referred to as mature cystic teratoma. It is an abnormal cyst that usually affects younger women and may grow to 6 inches in diameter. A dermoid cyst can contain other types of growths of body tissues such as fat and occasionally bone, hair, and cartilage. The ultrasound image of this cyst type can vary because of the spectrum of contents, but a CT scan and magnetic resonance imaging (MRI) can show the presence of fat and dense calcifications. These cysts can become inflamed. They can also twist around (a condition known as ovarian torsion), compromising their blood supply and causing severe abdominal pain.
Endometriomas or endometrioid cysts: Part of the condition known as endometriosis, this type of cyst is formed when endometrial tissue (the lining tissue of the uterus) is present on the ovaries. It affects women during the reproductive years and may cause chronic pelvic pain associated with menstruation. Endometriosis is the presence of endometrial glands and tissue outside the uterus. Women with endometriosis may have problems with fertility. Endometrioid cysts, often filled with dark, reddish-brown blood, may range in size from 0.75-8 inches.
Polycystic-appearing ovary: Polycystic-appearing ovary is diagnosed based on its enlarged size – usually twice that of normal – with small cysts present around the outside of the ovary. This condition can be found in healthy women and in women with hormonal (endocrine) disorders. An ultrasound is used to view the ovary in diagnosing this condition. Polycystic -appearing ovary is different from the polycystic ovarian syndrome (PCOS), which includes other symptoms and physiological abnormalities in addition to the presence of ovarian cysts. Polycystic ovarian syndrome involves metabolic and cardiovascular risks linked to insulin resistance. These risks include increased glucose tolerance, type 2 diabetes, and high blood pressure. Polycystic ovarian syndrome is associated with infertility, abnormal bleeding, increased incidences of miscarriage, and pregnancy-related complications. Polycystic ovarian syndrome is extremely common and is thought to occur in 4% -7% of women of reproductive age and is associated with an increased risk for endometrial cancer. The tests other than an ultrasound alone are required to diagnose polycystic ovarian syndrome.
Cystadenoma: A cystadenoma is a type of benign tumor that develops from ovarian tissue. They may be filled with a mucous-type fluid material. Cystadenomas can become very large and may measure 12 inches or more in diameter.
Ovarian Cysts Causes
The following are possible risk factors for developing ovarian cysts:
Oral contraceptive/birth control pill use decreases the risk of developing ovarian cysts because they prevent the ovaries from producing eggs during ovulation.
Ovarian Cysts Symptoms
Usually ovarian cysts do not produce symptoms and are found during a routine physical exam or are seen by chance on an ultrasound performed for other reasons. However, the following symptoms may be present:
Ovarian Cysts Diagnosis
The following tests may be performed to determine if a woman has an ovarian cyst or to help characterize the type of cyst that is present: It is important to ensure that pregnancy test is done.
Ovarian Cysts Medical Treatment
Oral contraceptives: Birth control pills may be helpful to regulate the menstrual cycle, prevent the formation of follicles that can turn into cysts, and possibly reduce the size of an existing cyst.
Pain relievers: Anti-inflammatory medication such as ibuprofen may help reduce pelvic pain. Narcotic pain medications by prescription may relieve severe pain caused by ovarian cysts.
Ovarian Cysts Surgery
Laparoscopic surgery: The surgeon makes small incisions through which a thin scope (laparoscope) can pass into the abdomen. The surgeon identifies the cyst through t he scope and may remove the cyst or take a sample from it.
Laparotomy: This is a more invasive surgery in which an incision is made through the abdominal wall in order to remove a cyst.
Surgery for ovarian torsion: An ovarian cyst may twist and cause severe abdominal pain as well as nausea and vomiting. This is an emergency, surgery is necessary to correct it.
Follow-up
Follow-up depends largely on the type of cyst that is present. Cysts in premenopausal women that show no evidence of cancer and are fewer than 4 inches in diameter may be observed for a period of time, while suspicious-appearing cysts may warrant immediate evaluation.
Prevention
Little medical information is available on the prevention of ovarian cysts. Smoking was not found to be a risk factor for their development. The use of oral contraceptive pills is associated with lower incidence or ovarian cysts.
Outlook
The outlook for a woman with an ovarian cyst depends on the type and size of cyst as well as her age. Benign (noncancerous) masses or cysts greatly outnumber malignant (cancerous) ones.
Age: The development of a functional ovarian cyst depends on hormonal stimulation of the ovary. A woman is more likely to develop a cyst if she is still menstruating and her body is producing the hormone estrogen. Postmenopausal women have a lower risk for developing ovarian cysts since they are no longer having menstrual periods. For this reason, many doctors recommend removal or biopsy of ovarian cysts in postmenopausal women, particularly if the cysts are larger than 1 -2 inches in diameter.
Cyst size: The size of the ovarian cyst relates directly to the rate at which they shrink. As a rule, functional cysts are 2 inches in diameter or smaller and usually have one fluid-filled area or bubble. The cyst wall is usually thin, and the inner side of the wall is smooth. An endovaginal ultrasound can reveal these features. Most cysts smaller than 2 inches in diameter are functional cysts. Surgery is recommended to remove any cyst larger than 4 inches in diameter.
Email: info@gyneclinics.com
Tel: 0207-117-6456, 0113-531-5007
Send download link to:
Email: info@gyneclinics.com
Tel: 0207-117-6456, 0113-531-5007
Every effort has been made to ensure that the details and factual matter on this website are as accurate as possible, however GyneClinics accepts no responsibility for decisions or treatment based upon information contained therein.

Hazel Lyons
Client Services Executive
A highly experienced and forward thinking professional with a proven track record in creating an outstanding patient experience and the delivery of exceptional customer service. Well versed in working with a variety of client groups, providing reception and administration duties and exceeding customer expectations.
A personable and passionate champion and brand role model of people, culture and values, with the ability to communicate, multi-task, influence and operate with integrity at all levels.

Hazel Lyons
Client Services Executive
A highly experienced and forward thinking professional with a proven track record in creating an outstanding patient experience and the delivery of exceptional customer service. Well versed in working with a variety of client groups, providing reception and administration duties and exceeding customer expectations.
A personable and passionate champion and brand role model of people, culture and values, with the ability to communicate, multi-task, influence and operate with integrity at all levels.

Mr Joe Daniels
MBBS, MSc, MRCPI, FRCOG
Consultant Urogynaecologist, Aesthetic Gynaecology
& Pelvic Floor Reconstruction
GMC Number 4349732
Mr Daniels has been practising obstetrics and gynaecology since 1989, and has been a consultant gynaecologist since 2003, within the NHS and private sector. He trained within the Cambridge Specialist Training rotation in aEast Anglia, and had his out of year and research experience at the Impetial College, London, where he studied the MRI appearances of women with pelvic floor problems, including Urinary Stress Incontinence. This generated his interest in how Laser Treatment can be helpful in improving pelvic health. Between 2011 and 2017, the bulk of his practice was in the private sector, with focus on Pelvic Floor Reconstruction and Aesthetic Gynaecology Since 2017, he returned to the NHS, and also continued with his private practice sessions in urogynaecology, pelvic floor reconstruction surgery and cosmetically related gynaecology.
He is currently Consultant Urogynaecologist at Airedale NHS Foundation Trust, Keighley, and provided support for the department at Mid-Yorkshire NHS at Pinderfields Hospital, Wakefield. He is also the Medical Director and Registered Manager at Regents Specialist Clinics. He also hold sessions at Harley Street, London, and Manchester .

Jaswinder Panesar
BDS (JUNE 1982), University of Dundee
Dental surgeon and facial aesthetics practitioner
Jas has Practiced as a principal dentist for 20 years in Halifax, 4 years in private dental care in Sowerby Bridge, the last seven years as a dental associate in Pudsey. He has 15 years of experience carrying out facial aesthetic procedures, including Botox injection and dermal fillers for the treatment of frown lines, facial wrinkle augmentation, restoring a smoother appearance. He also does Lip enhancement with fillers.

Kam Panesar
Aesthetics Skin Care Practitioner & Alternative Health Specialist
Kam specialises in Skin Care and Complementary Health. She Offers Anti-Ageing and Advanced skin care, for Scarring, Acne, young and mature skins. In addition to this her treatment. She is trained in Cool Laser Aesthetic treatment, cosmetic injections & dermal fillers
She is a practitioner is Stress Management techniques, including Anti-Stress Massage, Indian Head Massage , Hot Stones, Reflexology and Accupressure.

Cheryl Mason
Specialist Nurse and Complimentary Therapist
Cheryl’s background experience was in nursing, midwifery and pain management. She now qualified in and offers a range of complementary therapies at her clinics and at Regents Clinics. Her complimentary therapies involve a blend of acupuncture, hypnosis and therapeutic massage/body work techniques to suit the needs of the individual.
She has a Diploma and then Masters Degree from the esteemed Northern College of Acupuncture, York, where she has also been a guest lecturer. Between 2009 and 2015 Cheryl held a Lecturing and clinic supervisor post on the Acupuncture degree course at Leeds Beckett University (formerly Leeds Metropolitan University). During this time she gained the PGCHE teaching qualification. She also trains Physiotherapists, Osteopaths and Chiropractors in Acupuncture for the Acupuncture Association of Chartered Physiotherapists (AACP). Through her experience she has grown a deep respect for the powerful, yet gentle strength of Acupuncture to treat a wide range of conditions.
She is part way through a five year training in Masters degree in Osteopathic Medicine at the International College of Osteopathic Medicine in Surrey, and has expertise in Soft Tissue Massage and Chinese TuiNa Physical Therapy and yoga

Isabella Cavalli
Client Relationship and Business Development Executive
Isabella is passionate about aesthetics and help clients secure the best treatment for them. She is originally from Poland and moved to the UK around 16 years ago. Her background is in management and she has a Diploma in Fashion Textile and a BA from Leeds, which is where She lives currently with my twoand-a-half year old Akita called Rocky. She has always been obsessed with fashion, design, and beauty. She the creative director and founder of Satya& Ro and owns a social media agency alongside.

Dr Yosra Attia MB ChB
Medical Aesthetics Doctor
Dr Yos is an advanced aesthetic practitioner, medical grade skincare advisor, NHS doctor, GP registrar, and most importantly a 2020 mama (the best job of all).
She founded Skinpod in 2017 with the vision of breaking down the stigma behind aesthetic treatment – providing natural results that are bespoke and individual. With client education and involvement at the forefront of what She does. After graduating from University of Liverpool Medical school in 2015, She worked in multiple medical fields throughout her career – acute medicine, general surgery, obstetrics and gynaecology and even paediatrics to name a few. Currently working in general practice in West Yorkshire. After her foundation training – She had the privilege to be trained by various renowned aesthetic legends including Dr Riken at @avanti_aesthetics_academy in Harley Street, London.
She participates in Continuous Professional Development and believes that Confidence is Beautiful. Her aim is to help you become more confident in your own skin and wear it with pride.

Mr. Ammar Allouni
Consultant Plastic Surgeon (Breast & Body)
MB.BCh, MSc, MRCS Eng, FRCS (Plast)
GMC Number: 7034174
Mr. Allouni is a fully qualified and fully accredited UK plastic surgeon, on the GMC specialist register for Plastic and Reconstructive surgery. He is also a member of BAPRAS and CAPSCO. He qualified from Cairo University Hospitals in 2004 & started his plastic surgery training abroad before moving to the United Kingdom in 2008 to seek higher surgical training in plastic surgery. He has worked in multiple plastic surgery units both before & during higher plastic surgery training in Yorkshire and the Humber region.
Mr. Allouni has a special interest in breast aesthetics and reconstruction. He has completed advanced fellowship training at the Wythenshawe in Manchester. In his extensive experience in plastic surgery, he has worked closely with leading plastic and aesthetic surgeons in the UK and abroad. This was complemented by joining the CAPSCO Aesthetic Fellowship programme at Wood Medispa in Devon, one of the centres of excellence.
Mr. Allouni is an enthusiastic proponent of patient safety, and conducts his outpatients at Regents Clinics and under Kliniken, Harrogate. He also holds NHS appointment as a consultant plastic and reconstructive surgeon at Hull University Teaching Hospitals with a special interest in breast microsurgical reconstruction. He has a lovely wife and three daughters and tries to spend as much time with them as possible.
