Pelvic Inflammatory Disease
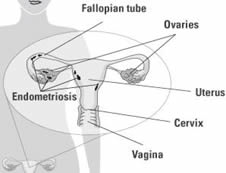
Pelvic inflammatory disease (PID) is a general term for infection of the upper genital tract, including the uterus, Fallopian tubes, and ovaries. It usually results from ascending infection from the cervix. It is a common and serious complication of some sexually transmitted diseases, especially chlamydia and gonorrhoea. It can damage the fallopian tubes and tissues in and near the uterus and ovaries. Untreated PID can lead to serious complications, including infertility, ectopic pregnancy, abscess formation and chronic pelvic pain.
- Genital chlamydial infection (Chlamydia trachomatis) and gonorrhoea (Neisseria gonorrhoeae) are currently the most common sexually transmitted infection diagnosed in the United Kingdom. However, several other organisms may be responsible, such as those commonly associated with bacterial vaginosis, e.g. Gardnerella vaginalis, Mycoplasma hominis, Mobiluncus and other anaerobes.
- Sexually Transmitted Infections are common in younger people, new sexual partner, multiple sexual partners, lack of barrier contraception, lower socio-economic group, termination of pregnancy and in the first 3-4 weeks after insertion of intrauterine contraceptive device (IUCD)
Presentation
Diagnosis of acute PID made only on clinical signs and positive swab results is 65-90% as accurate when compared to laparoscopic diagnosis. Many episodes of PID go unrecognised, as women often have absent, mild, or atypical symptoms.
Symptoms
The following features are suggestive of PID
- Lower abdominal pain – often on both sides.
- Deep painful sexual intercourse – deep dyspareunia.
- Abnormal vaginal bleeding (bleeding after sex, or heavy menstrual period or intermenstrual
- Pus-like vaginal or cervical discharge.
Signs
- Tenderness in the lower abdomen (usually on both sides).
- Cervical discharge that is a mixture of pus and mucous and inflammation and redness of the cervix will be seen on speculum examination.
- Tenderness when the cervix is moved during examination; and also tenderness in the region of the fallopian tubes and ovaries (adnexal) when internal pelvic vaginal examination is carried out, by the doctor.
- High temperature- fever – above 38°C (but the temperature may be normal).
Investigations
- Pregnancy test (pregnant women with PID should be admitted; ectopic pregnancy – pregnancy outside of the uterus – may be confused with PID).
- Cervical swabs for chlamydia and gonorrhoea: a positive result supports the diagnosis of PID, but a negative result does not exclude PID.
- Blood test may show signs of inflammation – pointing to a diagnosis of possible PID.
- Utrasound scanning may also be helpful, showing evidence of inflammation and swelling of the fallopian tubes and collection of inflammation tissue fluid.
- Laparoscopy with direct visualisation of the Fallopian tubes is the best single diagnostic test, but is an invasive procedure and therefore not necessary, when the diagnosis is clear.
- Urinalysis and urine culture: to exclude urinary tract infection; this may co-exist.
Management
- Provide adequate pain relief.
- If an intra-uterine contraceptive device – or coil – in present, this may need to be removed temporarily. The scientific evidence for whether an IUCD should be left in situ or removed is limited. Removal of the IUCD may be associated with better short-term clinical outcomes. The decision to remove the IUCD needs to be balanced against the risk of pregnancy in those who have had otherwise unprotected intercourse in the preceding seven days .
- Refer to a Sexual Health clinic, for a full sexually transmitted infection screen (HIV, etc.), contact tracing and treatment of sexual partners.
Antibiotic treatment
- The current outpatient treatment recommendation is ceftriaxone 500 mg as a single intramuscular (IM) dose, followed by doxycycline 100 mg orally twice-daily and metronidazole 400 mg twice-daily, for 14 days.
- Do not delay antibiotic treatment while waiting for the results of tests if PID is clinically suspected. It is likely that delayed treatment increases the risk of long -term complications, such as ectopic pregnancy, infertility and pelvic pain. Negative swabs do not exclude PID and therefore should not influence the decision to treat. Emphasise the importance of completing the course of antibiotics to reduce the risk of long -term complications.
- Broad-spectrum antibiotic treatment to cover trachomatis, N. gonorrhoeae and anaerobic infection is recommended.
- Other recommended regimes include:8
- Outpatient regimens:
- Ofloxacin 400 mg orally twice-daily plus oral metronidazole 400 mg twice-daily, for 14 days.9 This is not recommended if the woman is at high risk of gonococcal PID because of increasing quinolone resistance of gonorrhoea. Levofloxacin may be used as a once-daily, convenient alternative to ofloxacin.
- Severely ill patients:
- Intravenous (IV) therapy is recommended for patients with more severe clinical disease, e.g. pyrexia above 38°C, clinical signs of tubo-ovarian abscess, signs of pelvic peritonitis or pregnancy.
- Initial treatment with doxycycline, single-dose IV ceftriaxone and IV metronidazole, then change to oral doxycycline and metronidazole to complete 14 days of treatment.
- There is no evidence-based recommendation for treatment in pregnancy, but an empiric regimen might include IM ceftriaxone plus oral or IV erythromycin, with the possible addition of oral or IV metronidazole 500 mg three times daily in clinically severe disease. Any risk of this regimen is justified on the basis of need to provide therapy and low risk to the fetus.
- IV therapy should be continued for 24 hours after signs of clinical improvement.
Management of sexual partners
- Although most infected male partners have no symptoms, infection rates of 26-36% for Chlamydia trachomatis have been reported among partners.
- Patients should be advised to avoid unprotected intercourse until they, and their partner(s) have completed treatment and follow-up.
- Screen for other sexually transmitted infections, ideally at a Sexual Health clinic. All sexual partners within the previous six months (or the most recent sexual partner if there have been no sexual contacts within the previous six months) should be notified and offered screening for sexually transmitted infections.
- Sexual partners should be treated for chlamydial infection even if this is not identified on testing.
- Treatment for gonorrhoea only needs to be offered if gonorrhoeae is identified in the woman with PID or in her partner.
- Blind treatment for chlamydial infection and gonorrhoea should be given to partners who are unwilling to be screened.
Referral
Admission to secondary care (for IV antibiotics and/or further investigation) should be considered in the following situations:
- Diagnosis is uncertain, e.g. where appendicitis or ectopic pregnancy cannot be excluded.
- Severe symptoms or signs.
- Deteriorating clinical condition.
- No improvement with oral antibiotics within three days.
- Inability to tolerate oral treatment, e.g. due to nausea and vomiting.
- Presence of a tubo-ovarian abscess.
- Immunodeficiency, e.g. HIV infection, immunosuppression therapy.
Complications
- Infertility: the risk of infertility following PID is related to the number of episodes of PID and their severity.
- Ectopic pregnancy.
- Chronic pelvic pain.
- Perihepatitis (Fitz-Hugh and Curtis syndrome): causes right upper quadrant pain. Occurs in up to 10-20% of women with PID.
- Tubo-ovarian abscess.
- Reiter’s syndrome (reactive arthritis) – inflammation of the joints
- PID in pregnancy is associated with an increase in preterm delivery, and maternal and fetal morbidity. If this occurs around the time of birth, there could be neonatal chamydial infection – as perinatal transmission of trachomatis or N. gonorrhoeae can cause ophthalmia neonatorum. Also Chlamydial pneumonitis may also occur.
Prevention
- Limited evidence suggests that screening for chlamydia and treating identified infection prior to IUCD insertion reduces the risk of PID. Routine prophylactic antibiotics prior to IUCD insertion are not recommended.
- It has been recommended that testing for chlamydia be offered to women at increased risk of sexually transmitted infections and to all sexually active women aged under 25 years.