Uterine Fibroids
Uterine fibroids are the most common non-cancerous tumors in women of childbearing age. They are benign tumours that originate in the uterus (womb). Although they are composed of the same smooth muscle fibres as the uterine wall (myometrium), they are many times denser than normal myometrium. Uterine fibroids are usually round or semi-round in shape. The cause of fibroids is unknown. Risk factors include being of Afro-Caribbean origin or being overweight.
Causes and Risk Factors
We do not know exactly why women develop these tumours. Genetic abnormalities, alterations in growth factor (proteins formed in the body that direct the rate and extent of cell proliferation) expression, abnormalities in the vascular (blood vessel) system, and tissue response to injury have all been suggested to play a role in the development of fibroids.
Family history is a key factor, since there is often a history of fibroids developing in women of the same family. Race also appears to play a role. Women of African descent are two to three times more likely to develop fibroids than women of other races. Women of African ancestry also develop fibroids at a younger age and may have symptoms from fibroids in their 20s, in contrast to Caucasian women with fibroids, in whom symptoms typically occur during the 30s and 40s. Pregnancy and taking oral contraceptives both decrease the likelihood that fibroids will develop. Fibroids have not been observed in girls who have not reached puberty, but adolescent girls may rarely develop fibroids. Other factors that researchers have associated with an increased risk of developing fibroids include having the first menstrual period (menarche) prior to age 10, consumption of alcohol (particularly beer), uterine infections, and elevated blood pressure (hypertension).
Oestrogen tends to stimulate the growth of fibroids in many cases. During the first trimester of pregnancy, up to 30% of fibroids will enlarge and then shrink after the birth. In general, fibroids tend to shrink after menopause, but postmenopausal hormone therapy may cause symptoms to persist.
Overall, these tumours are fairly common and occur in up to 50% of all women. Most of the time, uterine fibroids do not cause symptoms or problems, and a woman with a fibroid is usually unaware of its presence
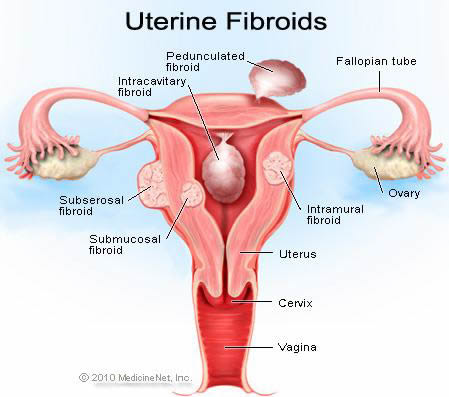
Types of Fibroids
Uterine fibroids are often described based upon their location within the uterus. Subserosal fibroids are located beneath the serosa (the lining membrane on the outside of the organ). These often appear localized on the outside surface of the uterus or may be attached to the outside surface by a pedicle. Submucosal (submucous) fibroids are located inside the uterine cavity beneath the lining of the uterus. Intramural fibroids are located within the muscular wall of the uterus.
Symptoms of Fibroids
What are the symptoms of uterine fibroids?
Most women with uterine fibroids have no symptoms.
However, abnormal uterine bleeding is the most common symptom of a fibroid. If the tumors are near the uterine lining, or interfere with the blood flow to the lining, they can cause heavy periods, painful periods, prolonged periods or spotting between menses. Women with excessive bleeding due to fibroids may develop iron deficiency anaemia. Uterine fibroids that are deteriorating can sometimes cause severe, localized pain.
Fibroids can also cause a number of symptoms depending on their size, location within the uterus, and how close they are to adjacent pelvic organs. Large fibroids can cause:
- pressure,
- pelvic pain,
- pressure on the bladder with frequent or even obstructed urination, and
- pressure on the rectum with pain during defecation.
While fibroids do not interfere with ovulation, some studies suggest that they may impair fertility and lead to poorer pregnancy outcomes. In particular, submucosal fibroids that deform the inner uterine cavity are most strongly associated with decreases in fertility.
- Pain in the back of the legs
- Pelvic pain or pressure
- Very heavy and prolonged menstrual periods
- Pressure on the bowel which may lead to constipation and/or bloating
- An enlarged abdomen (this may be mistaken for weight gain or pregnancy)
- Pain during sexual intercourse
- Pressure on the bladder which results in: a perpetual need to urinate, incontinence, or the inability to empty the bladder
Signs, Tests and Diagnosis
The following are the signs that can suggest fibroids
- Enlarged uterus (womb) – this sometimes will be large enough to be felt through the lower abdomen and sometimes appears like pregnant uterus . There may be change in the shape of your womb
- It can be difficult to diagnose fibroids, especially if you are extremely overweight.
- Uterine fibroids are diagnosed by pelvic exam and even more commonly by ultrasound. Often, a pelvic mass cannot be determined to be a fibroid on pelvic exam alone, and ultrasound is very helpful in differentiating it from other conditions such as ovarian tumours. Special scans – MRI and CT scans can play a role in diagnosing fibroids, but ultrasound is the simplest, cheapest, and almost without question the best technique for imaging the pelvis.
Treatment
Treatment depends on several things, including:
- Your age
- General health
- Severity of symptoms
- Type of fibroids
- Whether you are pregnant
- If you want children in the future
Some women may just need pelvic exams or ultrasounds every once in a while to monitor the fibroid’s growth.
Medical treatments
Non-surgical techniques are usually hormonal in nature and include the use of drugs that turn off the production of oestrogen from the ovaries (GnRH analogs). These medications are given for three to six months and induce a hypoestrogenic (low oestrogen) state. When successful, they can shrink the fibroids by as much as 50%. Side effects of these drugs are similar to the symptoms of the peri-menopause and can include hot flashes, sleep disturbance, vaginal dryness, and mood changes. Bone loss leading to osteoporosis after long-term (12+ months) use is the most serious complication. These drugs may also be used as preoperative treatment prior to undergoing surgical treatment of leiomyoma (fibroids).
Mifepristone is an antiprogestin drug that can shrink fibroids to an extent comparable to treatment with the GnRH analogs. This drug, sometimes known as the “morning-after pill” is also used to terminate early pregnancy. Treatment with mifepristone also reduced the bleeding associated with fibroids, but this treatment can be associated with adverse side effects such as overgrowth (hyperplasia) of the endometrium (uterine lining). Mifepristone is not approved by the US Food and Drug Administration (FDA) for the treatment of uterine leiomyomas, and the required dosages (different from those used for termination of early pregnancy) have not been determined.
Danazol is an androgenic steroid hormone that has been used to reduce bleeding in women with fibroids, since this drug causes menstruation to cease. However, danazol does not appear to shrink the size of fibroids. Danazol is also associated with significant side effects, including weight gain, muscle cramps, decreased breast size, acne, hirsutism (inappropriate hair growth), oily skin, mood changes, depression, decreased high density lipoprotein (HDL or ‘good cholesterol’) levels, and increased liver enzyme levels.
The administration of raloxifene (Evista) (a drug used to prevent and treat osteoporosis in postmenopausal women) has been shown to decrease the size of fibroids in postmenopausal women, but results with this therapy in premenopausal women have been conflicting.
Low dose formulations of oral contraceptives are also sometimes given to treat the abnormal bleeding associated with fibroids, but these do not shrink the fibroids themselves. Use of oral contraceptive pills has been associated with a decreased risk of developing fibroids, so some women may benefit from their use for this purpose
Surgical treatments
There are many ways of managing uterine fibroids. Surgical methods are the mainstay of treatment when treatment is necessary. Possible surgical interventions include Hysterectomy, or removal of the uterus (and the fibroids with it). Myomectomy is the selective removal of just the fibroids within the uterus. Myomectomy can be done through a laparoscope or with the standard open incision on the abdominal wall. Some treatments have involved boring holes into the fibroid with laser fibers, freezing probes (cryosurgery), and other destructive techniques that do not actually remove the tissue but try to destroy it in place. Surgery is necessary if there is suspicion of malignancy in any case of leiomyoma or uterine mass.
Another technique for treating fibroids is known as Uterine Artery Embolization (UAE). This technique uses small beads of a compound called polyvinyl alcohol, which are injected through a catheter into the arteries that feed the fibroid. These beads obstruct the blood supply to the fibroid and starve it of blood and oxygen. While this technique has not been in use long enough to evaluate long-term effects of UAE versus surgery, it is known that women undergoing UAE for fibroids have a shorter hospital stay than those having surgery but a greater risk of complications and readmissions to the hospital. Studies are underway to evaluate the long-term outcomes of UAE as opposed to surgical treatment. Uterine artery occlusion (UAO), which involves clamping the involved uterine arteries as opposed to injecting the polyvinyl alcohol beads, is currently under investigation as a potential alternative to UAE.
Uterine fibroids during pregnancy?
Uterine fibroids are identified in about 10% of pregnant women. Some studies have shown an increased risk of pregnancy complications in the presence of fibroids, such as first trimester bleeding, breech presentation, placental abruption, and problems during labour. Fibroids have also been associated with an increased risk of caesarean delivery. The size of the fibroid and its precise location within the uterus are likely to be important factors in determining whether a fibroid causes obstetric complications.
Do untreated uterine fibroids pose a risk?
For the most part, uterine fibroids that do not cause a problem for the woman can be left untreated. In some cases, even fibroids that are not causing symptoms require removal or at least close observation. Rapid growth is a reason to watch more carefully, since a rare cancerous form of fibroid (referred to as a leiomyosarcoma) is usually a fast-growing tumour, and it cannot be differentiated from a benign fibroid by ultrasound, MRI , or other imaging studies. However, this type of tumour occurs in less than 1% of uterine fibroids.
Another risk of leaving these tumours alone is that they sometimes grow to a size that eventually cause significant symptoms, thus requiring removal. If fibroids grow large enough, the surgery to remove them can become more difficult and risky. Occasionally, fibroids are the cause of recurrent miscarriages. If they are not removed in these cases, the woman may not be able to sustain a pregnancy
Complications of untreated fibroids may also include:
- Severe pain or excessively heavy bleeding that may require emergency surgery
- Twisting of the fibroid, which causes a blockage in nearby blood vessels feeding the tumor (surgery may be needed)
- Anemia (low red blood cell count) if the bleeding is very heavy
- Urinary tract infections, if pressure from the fibroid prevents the bladder from fully emptying
- Cancerous changes called leiomyosarcoma (rare)
In rare cases, fibroids may cause infertility. Fibroids may also cause complications if you become pregnant, although the risk is thought to be small:
- Some pregnant women with fibroids may deliver a premature baby because there is not enough room in the womb.
- A caesarean section may be needed if the fibroid blocks the birth canal or causes the baby to be in a dangerous position.
- Some pregnant women with fibroids have heavy bleeding immediately after giving birth.
UTERINE ARTERY EMBOLISATION (UAE)
Uterine Artery Embolisation (UAE) is a minimally invasive procedure that can be carried out through a small tube inserted into your groin. Through this tube, small plastic beads are injected into the arteries supplying blood to the fibroid. This blocks the arteries and causes the fibroid to shrink over the subsequent six months.
People who have UAE may suffer pain after the blood supply is removed, and strong painkillers are needed for about eight hours. There are some other complications that your specialist will be able to tell you about.
The advantage of UAE is that:
- it is successful in 95% of people who have heavy periods caused by fibroids
- serious complications are rare
- you only need to spend one night in hospital
- your womb and ovaries are not removed, so if you still want children this is possible
Further research needs to be carried out into the success rate of pregnancy after UAE. Sometimes, further embolisations or other procedures are needed after UAE. Your specialist will discuss this with you.
Myomectomy
Sometimes, the fibroids can be removed using a surgical procedure known as a myomectomy. However, the operation is not suitable for every type of fibroid. Your gynaecologist (specialist in the female reproductive system) will be able to tell you whether a myomectomy is possible and what the complications are.
When they are possible, myomectomies are very effective operations. However, in a quarter to a third of all people who have a myomectomy, the fibroids grow back again.









Leave a Reply
Want to join the discussion?Feel free to contribute!