Polycystic Ovarian Syndrome (PCOS)
Polycystic Ovarian Syndrome (PCOS) is the most common hormonal abnormality in reproductive-aged women affecting approximately 5-10% of population. It is the most common cause of infertility in women. The symptoms of PCOS may begin in adolescence with menstrual irregularities, or a woman may not know she has PCOS until later in life when symptoms and/or infertility occur.
The principal signs and symptoms of PCOS are related to menstrual disturbances and elevated levels of male hormones (androgens) and obesity. Menstrual disturbances can include delay of normal menstruation (primary amenorrhea), the presence of fewer than normal menstrual periods (oligomenorrhea), or the absence of menstruation for more than three months (secondary amenorrhea). Menstrual cycles may not be associated with ovulation (anovulatory cycles) and may result in heavy bleeding.
Symptoms related to elevated androgen levels include acne, excess hair growth on the body (hirsutism), and male-pattern hair loss.
Other signs and symptoms of PCOS include:
- obesity and weight gain, elevated insulin levels and insulin resistance
- oily skin, dandruff, skin discolorations,
- infertility,
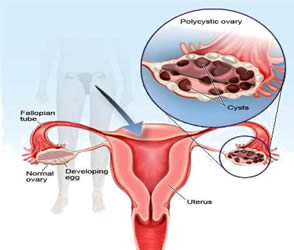
- multiple, small cysts in the ovaries.
Any of the above symptoms and signs may be absent in PCOS, with the exception of irregular or no menstrual periods. All women with PCOS will have irregular or no menstrual periods. Women who have PCOS do not regularly ovulate; that is, they do not release an egg every month. This is why they do not have regular periods and typically have difficulty conceiving.
PCOS involves a “vicious cycle” of hormonal imbalance that may begin with a oversensitivity of the pituitary to GnRH. The pituitary responds with an increase in LH secretion resulting in increased ovarian androgen production. Consequently, FSH production is inhibited thereby further preventing follicle development and ovulation. Additionally, oestrone proliferates the endometrium unopposed and increases the risk of endometrial hyperplasia. .
Causes
No one is quite sure what causes PCOS, and it is likely to be the result of a number of both genetic (inherited) as well as environmental factors. Women with PCOS often have a mother or sister with the condition, and researchers are examining the role that genetics or gene mutations might play in its development. The ovaries of women with PCOS frequently contain a number of small cysts, hence the name poly=many cystic ovarian syndrome. A similar number of cysts may occur in women without PCOS. Therefore, the cysts themselves do not seem to be the cause of the problem.
A malfunction of the body’s blood sugar control system (insulin system) is frequent in women with PCOS, who often have insulin resistance and elevated blood insulin levels, and researchers believe that these abnormalities may be related to the development of PCOS. It is also known that the ovaries of women with PCOS produce excess amounts of male hormones known as androgens. This excessive production of male hormones may be a result of or related to the abnormalities in insulin production.
Another hormonal abnormality in women with PCOS is excessive production of the hormone LH, which is involved in stimulating the ovaries to produce hormones and is released from the pituitary gland in the brain. Other possible contributing factors in the development of PCOS may include a low level of chronic inflammation in the body and fetal exposure to male hormones.
Clinical Presentation Explained
- a) Infertility:
Approximately 40% of female infertility factors result from ovulation problems. Women with PCOS may experience a wide range of ovulation problems, from oligoovulation to anovulation. In addition to anovulation, other factors appear to be involved, as these women may have a lower rate of conception in response to ovulation inducing agents (clomiphene citrate, gonadotropins) in comparison to women with hypothalamic amenorrhea (ovulation problem resulting from malfunction of this part of the brain). Many studies have also described the almost two fold increased miscarriage rate in PCOS, the mechanism of which is poorly understood.
- b) Abnormal Uterine Bleeding and Endometrial Hyperplasia
Due to chronic anovulation, women with PCOS usually have irregular mens trual bleeding. The high androgens levels can be converted peripherally to estrogens, particularly estrone, even in the absence of normal ovarian function. As a result, these women are exposed to continuous unopposed estrogen stimulation of the endometrium. Due to anovulation they are deficient in progesterone secretion, which is needed for endometrial differentiation and withdrawal bleeding. Thus, they are at risk for dysfunctional uterine bleeding and, ultimately, endometrial hyperplasia and/or carcinoma.
- c) Hyperandrogenism
The clinical features of androgen excess in women with PCOS include hirsutism, acne, male pattern balding (alopecia), and rarely signs of virilisation (maleness) including deepening of the voice, increased muscle mass, and clitoromegaly. Hirsutism occurs in approximately 70 – 80% of PCOS patients and is defined as the conversion of vellus (soft, unpigmented) to terminal (thick, pigmented) in a male pattern distribution along sex dependent regions, e.g. upper lip, around the nipple, and lower abdomen. Virilization is rare and women who present with rapidly progressive masculinizing signs should be evaluated for androgen tumors of the adrenal gland or ovary.
- d) Obesity
Obesity is a common, but not necessary, finding in at least 50% to 65% of women with PCOS. Patients usually have central (android) body fat distribution. Android obesity, which is characterized by increased waist-to-hip ratio (>0.80), is correlated with increased plasma testosterone, decreased sex-hormone-binding globulin, hyperinsulinemia, impaired glucose tolerance, and dyslipidemias.
- e) Insulin Resistance and Diabetes
Many women with PCOS exhibit insulin resistance and hyperinsulinemia. Although it is more commonly associated with obesity, it is also found in normal-weight women with PCOS. Because of insulin resistance, women with PCOS are at increased risk for impaired glucose tolerance and diabetes mellitus. A recent study determined that up to 40% of obese reproductive-age women with PCOS had impaired glucose tolerance and 7.5% had diabetes mellitus. In addition, 15% of normal – weight women with PCOS had impaired glucose tolerance and 1.5% had diabetes, a rate almost three-times that of the general population. The underlying reason for insulin resistance remains unclear. It has been reported that insulin resistance may be related to decreased insulin receptor processing (autophosphorylation) in about 50% of women with PCOS. If untreated, insulin resistance leads to diabetes in approximately one-third of patients.
- f) Possible predisposition to coronary heart disease:
Insulin resistance is a key finding along with elevated cholesterol, triglycerides, blood pressure, and waist circumference The presence of obesity, insulin resistance, and lipid abnormalities may predispose women with PCOS to coronary heart disease. Several studies have shown that women with PCOS have abnormal levels of LDL (“bad”) cholesterol and lowered levels of HDL (“good”) cholesterol in the blood.
DIAGNOSIS
PCOS is usually diagnosed clinically in women who present with oligomenorrhea (menstrual intervals >35 days), hyperandrogenism (elevated testosterone or hirsutism/acne) and obesity, after excluding other hormonal disorders. However, most women with PCOS do not exhibit all of these features and there is a considerable controversy about the definition and required criteria for the diagnosis. The new criteria include two of the following three signs: ovulation dysfunction; excessive hair growth and/or acne; and polycystic appearing ovaries on ultrasound. The diagnosis of PCOS does not require the presenceof polycystic ovaries on ultrasound since approximately 20% of fertile women may have polycystic appearing ovaries. Polycystic ovaries are present in more than 90% of women with PCOS but may sometimes be absent in women with all the other clinical characteristics of PCOS.
Polycystic ovary syndrome is primarily a clinical diagnosis, and laboratory findings should only be used to support the clinical testing and rule out other serious disorders. Evaluation should include measurement of thyroid-stimulating hormone (TSH), DHEA and testosterone, prolactin, and in some cases, morning 17alpha hydroxyprogesterone to rule out late-onset adrenal hyperplasia. The levels of testosterone that are highly elevated are not unusual with PCOS and call for additional evaluation. Additionally, levels of a hormone released by the pituitary gland in the brain (LH) that is involved in ovarian hormone production are elevated. Patients, regardless of age, with a greater than 3 month menstrual interval and/or an endometrial thickness of >= 7mm on ultrasound should undergo an endometrial biopsy to assess the risk of hyperplasia. Insulin resistance can best be evaluated by a 2 – hour glucose tolerance test (GTT).
MANAGEMENT
Weight reduction, diet and exercise are recommended for all women with PCOS. Some studies have also shown a 5-10% loss in body weight may result in a return of ovulatory cycles and a higher spontaneous pregnancy rate. However, it is very difficult for PCOS patients to loose weight. If body weight is reduced, it is also difficult to maintain due to a variety of reasons.
Monthly progesterone therapy can be used to prevent abnormal endometrial proliferation by inducing withdrawal bleeding. Another option for these women is to use low dose oral contraceptive pills (OCP) to regulate the menstrual cycle and provide contraception. Antiandrogens may be combined with oral contraceptive pills for the treatment of hirsutism and acne.
Also for acne or excess hair growth, a water pill (diuretic) called Spironolactone (Aldactone) may be prescribed to help reverse these problems. The use of spironolactone requires occasional monitoring of blood tests because of its potential effect on the blood potassium levels and kidney function. Eflornithine (Vaniqa) is a cream medication that can be used to slow facial hair growth in women. Electrolysis and over-the-counter depilatory creams are other options for controlling excess hair growth. Hair removal using laser and nonlaser light sources damages individual hair follicles so they do not grow back. This can be expensive and multiple treatments are needed. Laser removal can be combined with other medicines and hormones.
In patients desiring pregnancy, ovulation induction is often required usually with clomiphene citrate. Approximately 80% of women with PCOS ovulate in response to clomiphene, but only about 40% of them become pregnant. Most recently, an enzyme inhibitor of aromatase, letrozole, has been shown to have equal success as clomiphene with ovulation but less of a negative impact on endometrial proliferation. (Note: recently the drug manufacturer has advised against the use of letrozole in women pursuing pregnancy.). See other ovulation induction agents under “anovulation”. .
Insulin resistance has been implicated in the reproductive consequences of PCOS, namely infertility, miscarriage, and gestational diabetes. Multiple studies have supported the use of metform in to ameliorate these problems. Metformin “sensitizes” cells to insulin and PCOS patients are typically hyperinsulinemic (abnormally high level of insulin in the blood). It works by activating glucose transporters which allow passage of glucose into liver and muscle cells thereby decreasing peripheral insulin resistance. It is useful in reducing a number of the symptoms and complications of P COS,
being useful in the management of irregular periods, ovulation induction, weight loss, prevention of type 2 diabetes, and prevention of gestational diabetes mellitus in women with PCOS.
PCOS is sometimes treated with injectable follicle stimulating hormone. When Clomid or metformin fail to induce ovulation they are sometimes administered together. FSH is also sometimes combined with metformin.
Ovarian surgery has been an effective therapy for patients resistant to clomiphene citrate and/or letrozole. Laparoscopy with bilateral ovarian diathermy involves “drilling” holes in the ovary utilizing electrocautery or laser providing an approximate 84% ovulation induction rate and 56% pregnancy rate with maintenance of ovulation demonstrated for up to 20 years in the majority of patients.









Leave a Reply
Want to join the discussion?Feel free to contribute!